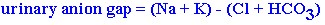
Renal tubular acidosis (RTA) is a group of disorders which manifests with a hyperchloremic metabolic acidosis caused by dysfunctional renal acid-base manipulation. The diagnosis of RTA should be strongly pursued in patients with a normal anion gap acidosis without renal impairment. A urinary pH of 5. 5 or greater supports the diagnosis once urinary tract infection has been excluded. Once negative urine cultures exclude infection as a possible etiology for the elevated urinary pH, the differential is between RTA and increased gastrointestinal bicarbonate loss. Calculation of the urinary anion gap will help distinguish between increased loss of bicarbonate from the gastrointestinal tract ( negative urinary anion gap) and distal RTA (positive urinary anion gap). The urinary anion gap is calculated as follows:
If urine pH > 6. 5:
If urine pH < 6. 5:
There are four distinct types of RTA:
TYPE I: This disorder occurs in the distal portion of the renal tubule and is associated with hypokalemia or normokalemia, normal anion gap acidosis and a urinary pH greater than 5. 6. Severe hypokalemia may stimulate ammonia synthesis enough to alkalinize the urine, so the diagnosis should be made only after adequate potassium supplementation has occurred. Type I RTA is often associated with nephrocalcinosis (multiple papillary calcifications noted on radiographs) which is rare in types II-IV. A definitive diagnosis can be made via the short ammonium chloride test. This test entails administering 0.1g/kg of ammonium chloride orally over 1-2 hours to produce a fall in plasma bicarbonate of 3-5 mmol/L. At this point a urinary pH greater than 5. 5 is diagnostic. The test is contraindicated in the presence of liver disease. Therapy involves correcting the underlying cause when possible or administering oral sodium bicarbonate at a dose of 1-2 mmol/kg/day.
CAUSES:
Familial, Sjogrens syndrome, systemic lupus erythematosus, primary biliary cirrhosis,
hepatic cirrhosis, chronic renal transplant rejection, hypergammaglobulinemia, medullary
sponge kidney, hypercalciuria, primary hyperparathyroidism, amphotericin B or toluene administration.
TYPE II: This disorder occurs in the proximal tubule and is an uncommon form of RTA in adults. Hypercalciuria and nephrocalcinosis are rare. The more common etiologies of proximal RTA are hypocalcemia, vitamin D deficiency and hyperparathyroidism but the list of possible etiologies is extensive (see below). Associated abnormalities include glycosuria, aminoaciduria and increased urinary phosphate and urate. Definitive diagnosis is made when the fractional excretion of bicarbonate exceeds 15% during a bicarbonate loading test. The fractional excretion of bicarbonate is calculated as follows:
The bicarbonate loading test is conducted as follows:
If the serum bicarbonate is greater than 20 mmol/L, ammonium chloride 0.1 g/kg is given orally over 1-2 hours. Next, sodium bicarbonate is given in a loading dose of [0. 5 x (30-plasma bicarbonate in mmol/L) x body weight in kg x 0.6] followed by 2 grams every15 minutes. The creatinine clearance and both the urine and plasma bicarbonate levels are determined hourly. In normal subjects, bicarbonate does not appear in the urine unless the plasma bicarbonate is greater than 26 mmol/L. In type II RTA the fractional excretion of bicarbonate is greater than 15% but in type I it is less than 5%.
If an underlying etiology can not be determined or is untreatable , type II RTA can be treated with sodium bicarbonate administration (3-5 mmol/kg/day) and potassium supplementation is often required. Metabolic bone disease is often responsive to therapy with vitamin D.
CAUSES:
Familial, cystinosis, Lowes syndrome, Wilsons disease, inherited fructose intolerance, primary hyperparathyroidism, vitamin D deficiency, vitamin D resistance, Cadmium poisoning, lead poisoning, Mercury poisoning, acetazolamide treatment, outdated tetracycline ingestion, multiple myeloma, amyloidosis, nephrotic syndrome, medullary cystic disease and renal transplant.
TYPE III: This disorder occurs in both the proximal and distal renal tubules. This is a rare variant of RTA seen almost exclusively in children.
TYPE IV: This disorder occurs in the distal tubule and is associated with hyperkalemia, mild metabolic acidosis and mild renal impairment. This is the most frequent type of RTA. Etiologies of type IV RTA are divided into those with hypoaldosteronism and those with intrinsic distal tubular disease. The most common etiology associated with this disorder is diabetes mellitus with mild renal impairment.
Diagnosis rests on showing failure to achieve a urinary pH lower than 5. 5 in the presence of acidosis and hyperkalemia greater than 5. 5 mmol/L. Measurement of plasma aldosterone and renin help differentiate between primary hypoaldosteronism, hyporeninemic hypoaldosteronism and renal tubular resistance to aldosterone. Therapy is usually aimed at correcting the serum potassium level and entails treatment with thiazide and loop diuretics to induce kaliuresis. Certain cases may require therapy with fluodrocortisone.
CAUSES:
Addisons disease, hyporeninemic hypoaldosteronism, interstitial nephritis, urinary tract obstruction, sickle cell disease, gout, systemic lupus erythematosus, renal transplant and medications (Amiloride, Spironolactone and Triamterene).